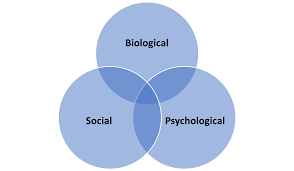
The Biopsychosocial Model represents a groundbreaking paradigm shift in modern healthcare, fundamentally transforming how medical professionals understand and treat patients. This comprehensive Biopsychosocial Model framework integrates biological, psychological, and social factors to provide holistic patient care that addresses the complete human experience rather than isolated symptoms. Developed by psychiatrist George Engel in 1977, the Biopsychosocial Model emerged as a direct response to the limitations of traditional biomedical approaches. This revolutionary Biopsychosocial Model recognizes that human health and illness result from complex interactions between multiple interconnected systems, requiring comprehensive assessment and treatment strategies. Healthcare professionals worldwide increasingly adopt the Biopsychosocial Model to deliver more effective, patient-centered care that addresses root causes rather than symptoms alone. This evidence-based Biopsychosocial Model approach has demonstrated superior outcomes across various medical specialties, from primary care to psychiatric treatment and chronic disease management.
Historical Development and Origins of the Biopsychosocial Model
The Medical Revolution That Changed Healthcare Forever
Dr. George Engel introduced the Biopsychosocial Model during the 1970s as medical science began recognizing the significant limitations of purely biomedical approaches. The traditional Biopsychosocial Model predecessor focused exclusively on biological factors, often overlooking crucial psychological and social determinants of health and illness. Engel’s innovative Biopsychosocial Model challenged the reductionist medical thinking that dominated healthcare for centuries. This paradigm-shifting Biopsychosocial Model proposed that effective healthcare requires understanding patients as complete human beings embedded within complex social systems rather than biological machines requiring mechanical repairs. The scientific community initially resisted the Biopsychosocial Model due to its departure from established medical traditions. However, mounting research evidence supporting the Biopsychosocial Model effectiveness gradually convinced healthcare professionals to embrace this comprehensive approach to patient care and treatment planning.
Evolution and Refinement of the Biopsychosocial Model Framework
Over decades, researchers and clinicians have continuously refined the Biopsychosocial Model to incorporate new scientific discoveries and clinical insights. Modern versions of the Biopsychosocial Model include environmental factors, cultural considerations, and spiritual dimensions that influence health outcomes and treatment effectiveness. Contemporary applications of the Biopsychosocial Model extend beyond individual patient care to include public health initiatives, healthcare policy development, and medical education curricula. This expanded Biopsychosocial Model scope reflects growing recognition that health and illness are inherently multidimensional phenomena requiring comprehensive understanding and intervention.
Core Components of the Biopsychosocial Model
Biological Factors: The Foundation of Physical Health
The biological component of the Biopsychosocial Model encompasses genetic predispositions, neurochemical imbalances, hormonal fluctuations, and physiological processes that directly impact health outcomes. This fundamental Biopsychosocial Model element includes infectious diseases, chronic conditions, medication effects, and age-related changes that influence patient wellbeing and treatment responses. Healthcare providers utilizing the Biopsychosocial Model conduct comprehensive biological assessments including laboratory tests, imaging studies, and physical examinations. This thorough Biopsychosocial Model evaluation ensures that underlying medical conditions receive appropriate attention while considering their interactions with psychological and social factors. Modern applications of the Biopsychosocial Model incorporate advances in genomics, personalized medicine, and precision healthcare approaches. This scientific evolution enhances the Biopsychosocial Model biological component by providing deeper insights into individual genetic vulnerabilities and treatment responsiveness patterns.
Psychological Factors: The Mind-Body Connection
The psychological dimension of the Biopsychosocial Model addresses cognitive patterns, emotional regulation, behavioral habits, and mental health conditions that significantly impact physical health outcomes. This crucial Biopsychosocial Model component recognizes that thoughts, feelings, and behaviors directly influence immune function, pain perception, and recovery processes. Clinical applications of the Biopsychosocial Model psychological component include assessment of depression, anxiety, stress levels, coping mechanisms, and personality factors. Healthcare providers using the Biopsychosocial Model evaluate how psychological states contribute to symptom development, treatment adherence, and overall health outcomes. Research supporting the Biopsychosocial Model psychological component demonstrates clear connections between mental health and physical wellbeing. This evidence-based Biopsychosocial Model approach has revolutionized treatment of chronic pain, cardiovascular disease, autoimmune conditions, and many other health challenges.
Social Factors: Environmental Influences on Health
The social component of the Biopsychosocial Model examines family dynamics, cultural background, socioeconomic status, social support systems, and environmental stressors affecting health outcomes. This comprehensive Biopsychosocial Model dimension recognizes that individual health cannot be separated from social context and community influences. Healthcare professionals implementing the Biopsychosocial Model assess housing conditions, employment status, educational background, and relationship quality as essential health determinants. This holistic Biopsychosocial Model approach addresses social isolation, discrimination, poverty, and other social factors that significantly impact health outcomes. Community health initiatives based on the Biopsychosocial Model focus on addressing social determinants of health through policy changes, community programs, and environmental improvements. This population-level Biopsychosocial Model application has demonstrated significant improvements in public health outcomes and healthcare equity.
Clinical Applications of the Biopsychosocial Model
Primary Care Integration and Implementation
Primary care physicians increasingly utilize the Biopsychosocial Model to provide comprehensive patient care that addresses multiple health determinants simultaneously. This integrated Biopsychosocial Model approach enables early identification of psychological and social factors that may complicate medical treatment or influence health outcomes. Family medicine practitioners applying the Biopsychosocial Model conduct thorough assessments that include screening for mental health conditions, social stressors, and environmental factors. This comprehensive Biopsychosocial Model evaluation improves diagnostic accuracy and enables more effective treatment planning that addresses root causes rather than symptoms alone.
Mental Health Treatment and Psychiatric Care
Mental health professionals extensively employ the Biopsychosocial Model to understand and treat psychiatric conditions within their complete context. This holistic Biopsychosocial Model approach recognizes that mental health disorders result from complex interactions between genetic vulnerabilities, psychological factors, and social circumstances. Psychiatrists and psychologists using the Biopsychosocial Model develop comprehensive treatment plans that may include medication management, psychotherapy, and social interventions. This integrated Biopsychosocial Model approach has demonstrated superior outcomes compared to single-modality treatments for depression, anxiety, bipolar disorder, and other mental health conditions.
Chronic Disease Management and Care
Healthcare teams managing chronic diseases increasingly adopt the Biopsychosocial Model to address the complex factors influencing disease progression and treatment adherence. This comprehensive Biopsychosocial Model approach recognizes that conditions like diabetes, heart disease, and arthritis require attention to psychological and social factors alongside medical treatment. Chronic disease programs based on the Biopsychosocial Model include patient education, stress management training, social support development, and lifestyle modification interventions. This holistic Biopsychosocial Model approach has demonstrated significant improvements in disease outcomes, quality of life, and healthcare utilization patterns.
Benefits and Advantages of the Biopsychosocial Model
Improved Patient Outcomes and Treatment Effectiveness
Research consistently demonstrates that healthcare approaches based on the Biopsychosocial Model achieve superior patient outcomes compared to traditional biomedical methods. This evidence-based Biopsychosocial Model approach reduces symptom severity, improves functional status, and enhances overall quality of life across diverse patient populations. Patients receiving care based on the Biopsychosocial Model report higher satisfaction levels, improved treatment adherence, and better therapeutic relationships with healthcare providers. This patient-centered Biopsychosocial Model approach addresses individual needs and preferences while maintaining scientific rigor and clinical effectiveness.
Enhanced Healthcare Provider Satisfaction and Effectiveness
Healthcare professionals utilizing the Biopsychosocial Model report increased job satisfaction and reduced burnout rates compared to those using traditional biomedical approaches. This comprehensive Biopsychosocial Model framework provides clinicians with tools to address complex patient presentations that resist conventional treatment approaches. Medical education programs incorporating the Biopsychosocial Model produce graduates who are better prepared to handle the complexities of modern healthcare. These Biopsychosocial Model-trained providers demonstrate superior clinical reasoning skills and more effective patient communication abilities.
Cost-Effectiveness and Healthcare Resource Utilization
Healthcare systems implementing the Biopsychosocial Model demonstrate improved cost-effectiveness through reduced hospitalization rates, decreased emergency department visits, and more efficient resource utilization. This economic Biopsychosocial Model advantage results from addressing root causes rather than treating symptoms repeatedly. Preventive interventions based on the Biopsychosocial Model reduce long-term healthcare costs by identifying and addressing risk factors before they develop into serious health conditions. This proactive Biopsychosocial Model approach represents a fundamental shift toward sustainable healthcare delivery that benefits both patients and healthcare systems.
Challenges and Limitations of the Biopsychosocial Model
Implementation Barriers and Practical Constraints
Despite its proven effectiveness, implementing the Biopsychosocial Model faces significant challenges including time constraints, resource limitations, and training requirements. Healthcare providers may struggle to conduct comprehensive Biopsychosocial Model assessments within current healthcare delivery structures that prioritize efficiency over thoroughness. Insurance reimbursement systems often fail to adequately support Biopsychosocial Model approaches that require extended evaluation times and multidisciplinary coordination. These financial constraints limit Biopsychosocial Model adoption despite clear evidence of its clinical and economic benefits over traditional approaches.
Training and Education Requirements
Effective implementation of the Biopsychosocial Model requires specialized training and ongoing education for healthcare providers across multiple disciplines. Medical schools and residency programs must integrate Biopsychosocial Model principles into their curricula to prepare future healthcare professionals for comprehensive patient care. Continuing education programs focused on the Biopsychosocial Model help practicing clinicians develop necessary skills and knowledge. These educational initiatives ensure consistent Biopsychosocial Model application and maintain high standards of patient care across healthcare settings.
Future Directions and Innovations in the Biopsychosocial Model
Technology Integration and Digital Health Solutions
Emerging technologies offer exciting opportunities to enhance Biopsychosocial Model implementation through digital health platforms, artificial intelligence, and telemedicine solutions. These innovative Biopsychosocial Model applications can streamline comprehensive assessments while maintaining the holistic approach that defines this healthcare paradigm. Mobile health applications based on the Biopsychosocial Model enable continuous monitoring of biological, psychological, and social factors that influence health outcomes. These technological Biopsychosocial Model innovations provide real-time data to support clinical decision-making and patient self-management strategies.
Research and Evidence Development
Ongoing research continues to refine and validate Biopsychosocial Model applications across diverse patient populations and healthcare settings. Large-scale studies examining Biopsychosocial Model effectiveness provide compelling evidence for its adoption in mainstream healthcare delivery systems. Future research directions include investigating optimal Biopsychosocial Model implementation strategies, identifying patient populations that benefit most from this approach, and developing standardized assessment tools. This expanding Biopsychosocial Model evidence base supports continued adoption and refinement of this comprehensive healthcare approach.

[…] 3. Biopsychosocial Model Definition […]